COPD Pathogenesis
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is characterized by persistent airflow limitation and a complex inflammatory response in the airways and lung parenchyma. This review examines the molecular and cellular mechanisms underlying COPD pathogenesis, with particular focus on inflammatory pathways, immune responses, and tissue remodeling.
Oxidative Stress and Initial Triggers:
Environmental Triggers and Oxidative Stress
1.Cigarette Smoke Components
○ Direct oxidants
○ Free radicals
○ Reactive oxygen species (ROS)
○ Reactive nitrogen species (RNS)
2.Cellular Response to Oxidative Stress
○ Mitochondrial dysfunction
○ DNA damage
○ Protein modification
○ Lipid peroxidation
○ NF-κB activation
3.Antioxidant Systems
○ Nuclear factor erythroid 2-related factor 2 (Nrf2)
○ Superoxide dismutase
○ Glutathione systems
○ Catalase
○ Impairment in COPD
Epithelial Cell Response
1.Barrier Dysfunction
○ Tight junction disruption
○ Increased permeability
○ Mucus hypersecretion
○ Ciliary dysfunction
2.Inflammatory Mediator Production
○ IL-1β
○ IL-6
○ IL-8 (CXCL8)
○ TNF-α
○ Growth factors
3.Cell Death Mechanisms
○ Apoptosis
○ Necrosis
○ Necroptosis
○ Pyroptosis
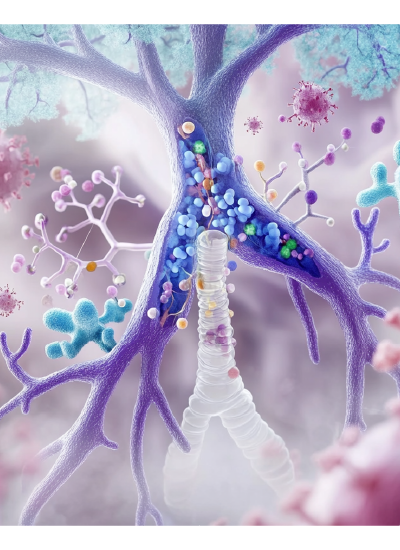

Innate Immune Response
Neutrophilic Inflammation
1.Neutrophil Recruitment
○ CXCL8 (IL-8) signaling
○ Leukotriene B4
○ Complement activation
○ Adhesion molecule expression
2.Neutrophil Activity
○ Protease release
■ Neutrophil elastase
■ Cathepsin G
■ Matrix metalloproteinases
■ Proteinase 3
○ Oxidant generation
■ NADPH oxidase activation
■ Myeloperoxidase release
■ NET formation
3.Tissue Damage Mechanisms
○ Direct proteolytic damage
○ Oxidative injury
○ ECM degradation
○ Mucus hypersecretion
Macrophage Activation
1.Recruitment and Differentiation
○ Monocyte recruitment
○ Alveolar macrophage proliferation
○ M1/M2 polarization
○ Activation states
2.Inflammatory Mediator Production
○ TNF-α
○ IL-1β
○ IL-6
○ CXCL8
○ MMPs
3.Phagocytic Function
○ Impaired bacterial clearance
○ Defective efferocytosis
○ Enhanced inflammatory response


Innate Lymphoid Cells
1.ILC1s
○ IFN-γ production
○ TNF-α release
○ Tissue destruction
2.ILC3s
○ IL-17 production
○ IL-22 release
○ Neutrophil recruitment
Adaptive Immune Response
T Cell Responses
1.CD8+ T Cells
○ Cytotoxic activity
○ Perforin/granzyme release
○ IFN-γ production
○ Tissue destruction
2.CD4+ T Cells
○ TH1 responses
■ IFN-γ production
■ Macrophage activation
○ TH17 responses
■ IL-17 production
■ Neutrophil recruitment
3.Regulatory T Cells
○ Reduced function
○ Impaired immunoregulation
○ Inflammation persistence

B Cell Responses
1.Lymphoid Follicle Formation
○ CXCL13 production
○ B cell recruitment
○ Germinal center formation
2.Autoantibody Production
○ Anti-elastin antibodies
○ Anti-epithelial antibodies
○ Complement activation
3.Local Antibody Production
○ IgA deficiency
○ Altered mucosal immunity
○ Bacterial colonization
Inflammatory Mediators and Signaling Pathways
Cytokine Networks
1.Pro-inflammatory Cytokines
○ TNF-α
■ Cell activation
■ Tissue destruction
■ Inflammation amplification
○ IL-1β
■ Acute phase response
■ Inflammatory cell recruitment
■ Matrix degradation
○ IL-6
■ Systemic inflammation
■ Acute phase proteins
■ B cell activation
2.Chemokines
○ CXCL8 (IL-8)
○ CXCL1
○ CCL2
○ CXCL10

Lipid Mediators
1.Leukotrienes
○ LTB4 production
○ Neutrophil recruitment
○ Inflammation amplification
2.Prostaglandins
○ PGE2 effects
○ Inflammatory modulation
○ Tissue repair
Growth Factors
1.TGF-β
○ Small airway fibrosis
○ Matrix production
○ Epithelial-mesenchymal transition
2.VEGF
○ Vascular remodeling
○ Emphysema development
○ Tissue repair


Protease-Antiprotease Imbalance
Proteases
1.Neutrophil Elastase
○ Elastin degradation
○ Mucus secretion
○ Inflammation amplification
2.Matrix Metalloproteinases
○ MMP-9
○ MMP-12
○ ECM degradation
3.Cathepsins
○ Tissue destruction
○ Matrix degradation
○ Inflammation modulation
Antiproteases
1.α1-Antitrypsin
○ Elastase inhibition
○ Anti-inflammatory effects
○ Deficiency consequences
2.TIMP Production
○ MMP inhibition
○ Tissue protection
○ Remodeling regulation


Tissue Remodeling and Repair
Airway Remodeling
1.Small Airway Changes
○ Fibrosis
○ Smooth muscle hypertrophy
○ Goblet cell hyperplasia
2.ECM Alterations
○ Collagen deposition
○ Elastin degradation
○ Proteoglycan changes
Emphysema Development
1.Alveolar Destruction
○ Loss of attachments
○ Reduced elastic recoil
○ Air trapping
2.Failed Repair
○ Stem cell dysfunction
○ Senescence
○ Impaired regeneration


Systemic Manifestations
Systemic Inflammation
1.Inflammatory Mediators
○ Acute phase proteins
○ Pro-inflammatory cytokines
○ Oxidative stress markers
2.Metabolic Effects
○ Muscle wasting
○ Bone density loss
○ Cardiovascular complications
Cellular Senescence
1.Mechanisms
○ Telomere shortening
○ DNA damage
○ Oxidative stress
○ Mitochondrial dysfunction
2.Consequences
○ SASP production
○ Tissue dysfunction
○ Impaired repair


Eosinophilic COPD and Biological Therapies
Type 2 Inflammation in COPD
1.Characteristics of Eosinophilic COPD
○ Blood eosinophil counts ≥300 cells/µL
○ Increased tissue eosinophilia
○ Enhanced IL-4, IL-5, IL-13 expression
○ Overlapping features with asthma
○ Better response to corticosteroids
○ Frequent exacerbations
2.Pathophysiological Mechanisms
○ Epithelial alarmin production (TSLP, IL-33, IL-25)
○ ILC2 activation and proliferation
○ TH2 cell differentiation
○ Eosinophil recruitment and activation
○ Tissue remodeling
3.Clinical Significance
○ Distinct COPD phenotype
○ Predictive biomarker for exacerbations
○ Treatment response indicator
○ Therapeutic target selection
Targeted Biological Therapies
1.Anti-IL-4Rα (Dupilumab)
○ Mechanism of Action
■ Blocks IL-4 and IL-13 signaling
■ Reduces type 2 inflammation
■ Decreases eosinophil recruitment
■ Modifies tissue remodeling
○ Clinical Evidence
■ Reduction in exacerbations
■ Improvement in lung function
■ Better symptom control
■ Safety profile
○ Patient Selection
■ Blood eosinophil levels
■ Exacerbation history
■ Type 2 inflammatory markers
2.Anti-IL-5 (Mepolizumab)
○ Mechanism of Action
■ Targets IL-5 directly
■ Reduces eosinophil survival
■ Decreases eosinophil recruitment
■ Modulates tissue inflammation
○ Clinical Applications
■ Exacerbation reduction
■ Steroid-sparing effects
■ Impact on lung function
■ Quality of life improvements
○ Biomarker Guidance
■ Blood eosinophil thresholds
■ Previous exacerbation history
■ Response prediction
3.Anti-TSLP (Tezepelumab)
○ Mechanism of Action
■ Blocks TSLP signaling
■ Reduces multiple inflammatory pathways
■ Affects both innate and adaptive immunity
■ Broader anti-inflammatory effects
○ Potential Benefits
■ Upstream pathway modification
■ Multiple cell type effects
■ Exacerbation reduction
■ Lung function improvement
○ Target Population
■ Less dependent on eosinophil counts
■ Multiple inflammatory phenotypes
■ Frequent exacerbators
4.Anti-IL-33 Antibodies
○ Mechanism of Action
■ Blocks IL-33 signaling
■ Reduces ILC2 activation
■ Decreases type 2 inflammation
■ Modifies tissue responses
○ Development Status
■ Clinical trial results
■ Safety observations
■ Efficacy markers
○ Potential Applications
■ Early intervention
■ Prevention of exacerbations
■ Tissue remodeling modification

Integration with Standard Therapy
1.Combination Approaches
○ With inhaled corticosteroids
○ With bronchodilators
○ Optimization strategies
○ Sequential therapy
2.Treatment Selection
○ Biomarker guidance
○ Clinical characteristics
○ Cost considerations
○ Risk-benefit assessment
Future Directions in Biological Therapy
1.Emerging Targets
○ Novel cytokine pathways
○ Combined pathway inhibition
○ Tissue-specific approaches
○ Personalized selection
2.Research Needs
○ Predictive biomarkers
○ Response durability
○ Long-term outcomes
○ Cost-effectiveness

Clinical Implications and Therapeutic Targeting
Biomarker Development
1.Inflammatory Markers
○ Blood neutrophils
○ CRP
○ Fibrinogen
○ Pro-inflammatory cytokines
2.Tissue Destruction Markers
○ Desmosine
○ MMPs
○ ECM fragments
Therapeutic Approaches
1.Anti-inflammatory Strategies
○ Phosphodiesterase-4 inhibitors
○ CXCR2 antagonists
○ p38 MAPK inhibitors
2.Protease Inhibition
○ Neutrophil elastase inhibitors
○ MMP inhibitors
○ α1-antitrypsin augmentation
3.Oxidative Stress Reduction
○ Nrf2 activators
○ Antioxidant therapy
○ Mitochondrial targets


Future Directions
Emerging Therapeutic Targets
1.Novel Pathways
○ Senescence targeting
○ Stem cell therapy
○ Tissue regeneration
2.Combination Approaches
○ Multiple pathway inhibition
○ Personalized medicine
○ Disease modification
Research Needs
1.Early Disease Mechanisms
○ Initial triggers
○ Progression factors
○ Prevention strategies
2.Biomarker Development
○ Disease phenotyping
○ Treatment response
○ Progression markers

Conclusion
COPD pathogenesis involves complex interactions between environmental triggers, innate and adaptive immune responses, and tissue repair mechanisms. Understanding these pathways is crucial for developing effective therapeutic strategies. The heterogeneity of COPD suggests that personalized approaches targeting specific pathogenic mechanisms may be necessary for optimal treatment outcomes.